Research
Championing Excellence in Biomedical Research
 What makes females so susceptible to hypertension-related mortality? ROAR aims to
advance our understanding of sex-specific mechanisms that control blood pressure to
limit cardiovascular risk.
What makes females so susceptible to hypertension-related mortality? ROAR aims to
advance our understanding of sex-specific mechanisms that control blood pressure to
limit cardiovascular risk.
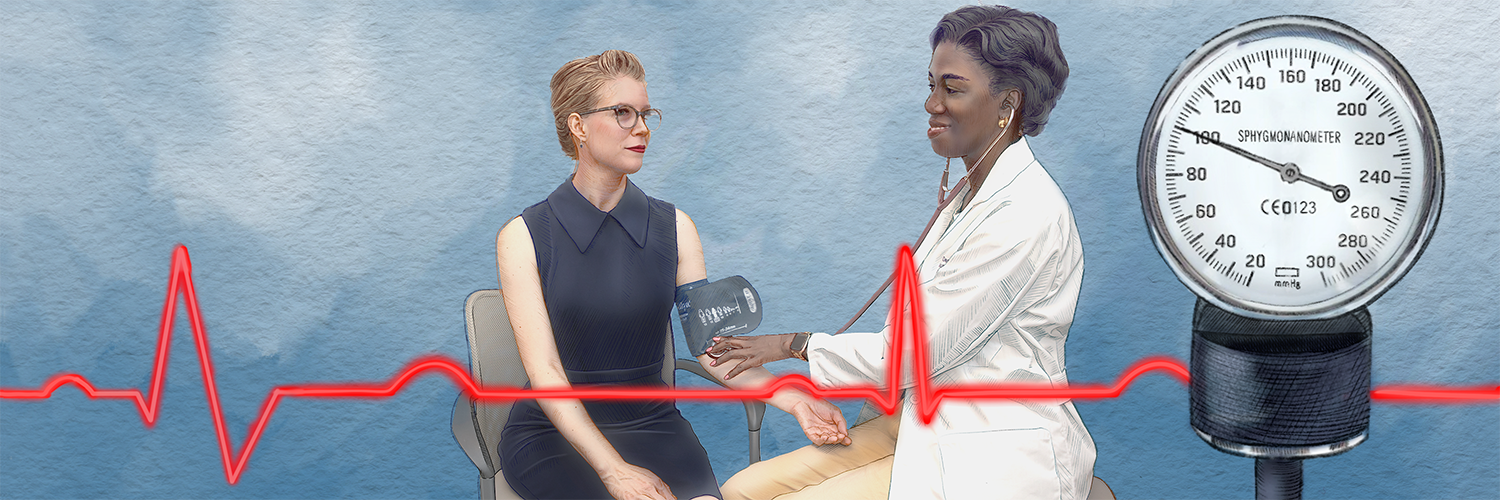
Heart disease remains the leading cause of death for men and women in the US. Hypertension is a major modifiable risk factor for CVD, and it has been suggested that eliminating hypertension would reduce CVD mortality by 30% in men and 38% in women. Although young women are considered “protected” from hypertension and the associated cardiovascular risk relative to age-matched men, the elimination of hypertension is projected to have a larger impact on CVD mortality in women. As an NIH-supported Specialized Center Of Research Excellence, ROAR is part of a national consortium that aims to advance Sex As a Biological Variable (SABV) to improve biomedical research and ultimately, clinical care for both men and women.
Background
The Problem
According to the latest guidelines, about 47% of U.S. adults have high blood pressure. In around 85% of cases, the cause is unknown, and only about 50% of those on medication manage to control it.
The rural South has the highest risk of death from high blood pressure, and certain groups of women are especially vulnerable to developing high blood pressure and heart disease. A critical barrier to limiting premature death from Cardiovascular Disease is a lack of awareness surrounding the risks.
Research is needed to advance our understanding of sex-specific mechanisms that control blood pressure (BP) to limit CV risk. The ROAR research projects are designed to improve scientific knowledge regarding the mechanisms controlling BP in (1) response to a high-fat diet and increases in obesity in males and females and (2) the role of autoimmunity in promoting hypertension and Cardiovascular risk. All three projects include both preclinical and clinical experiments to address important gaps in our understanding of SABV in CVD.
The Partnership
ROAR is a collaborative project spanning 3 universities including Augusta University, University of South Carolina, and The University of Mississippi Medical Center.
Researchers aim to provide novel insights into the mechanisms controlling blood pressure in females vs. males to ultimately improve clinical care.
Scientific Projects
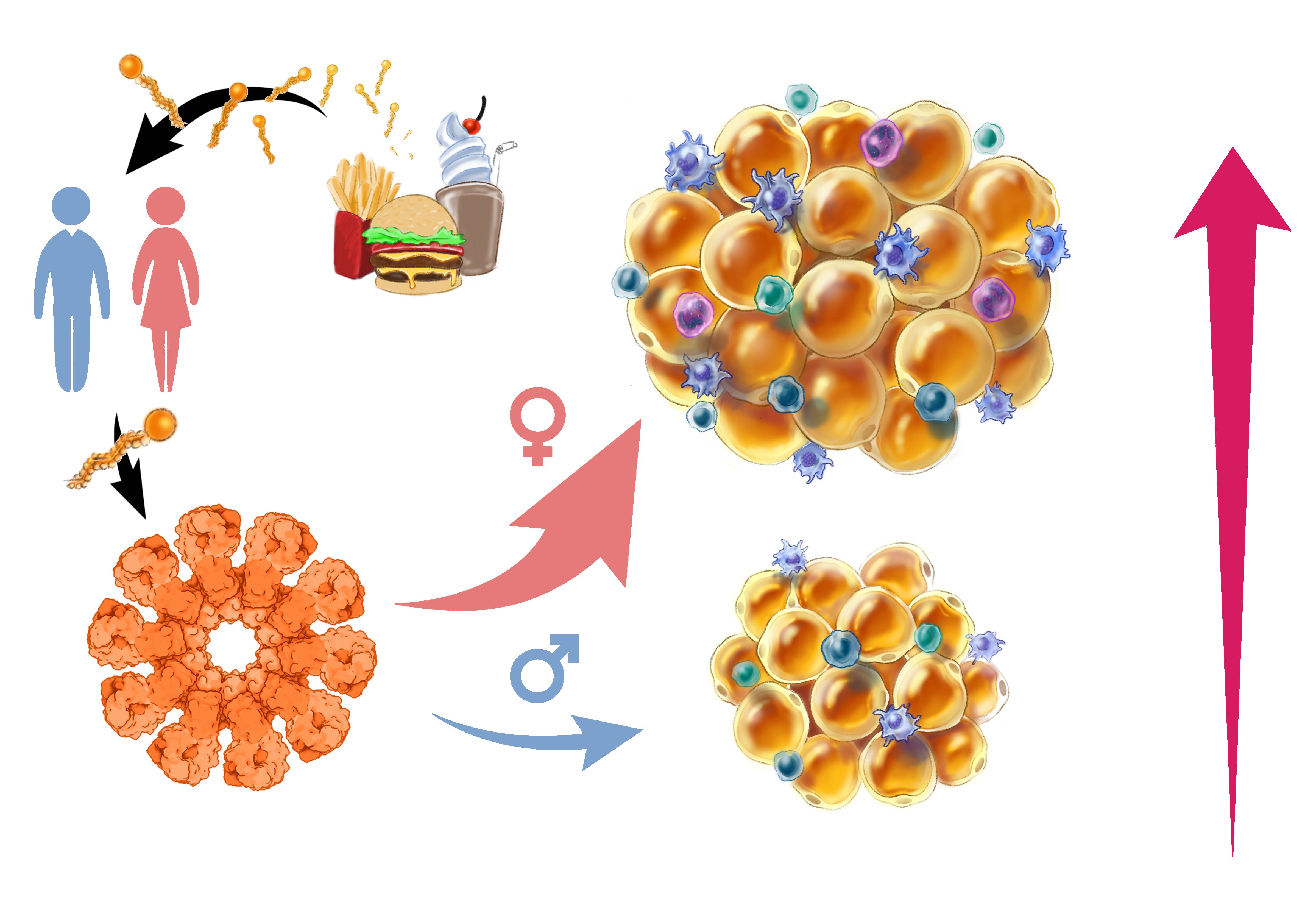
Mechanisms Driving Enhanced Susceptibility of Females versus Males to High-Fat Diet-Induced Increases in High Blood Pressure
Hypertension, which is linked to diets high in saturated fats, is the world’s largest contributing factor to disease and mortality. This study examines how such diets activate the immune system, increasing fat and blood pressure, especially in women.
Focusing on the NLRP3 protein, researchers will compare its levels in male and female rats and humans. The project aims to understand why women might be more affected and how immune cells contribute to fat and inflammation differently between sexes. The goal is to find better treatments for hypertension by targeting its root causes. View Full Graphic Abstract
The Impact of Obesity and Leptin on Immune System Dysfunction and Hypertension in Females with Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that mainly affects women and leads to the body's immune system attacking itself, causing chronic inflammation, hypertension, and heart disease. SLE patients often have higher rates of obesity and abnormal fat distribution, even if they are not overweight. They also have elevated levels of leptin, a hormone involved in fat regulation.
This project aims to understand how obesity and leptin contribute to SLE and hypertension.
Using two mouse models, researchers will investigate how increased fat worsens SLE
and whether reducing fat or certain immune cells in fat can slow disease progression.
They will also explore if leptin directly affects immune cells and if its impact on
the brain influences SLE. The findings could reveal new ways obesity and leptin contribute
to immune dysfunction and hypertension in SLE. View Full Graphic Abstract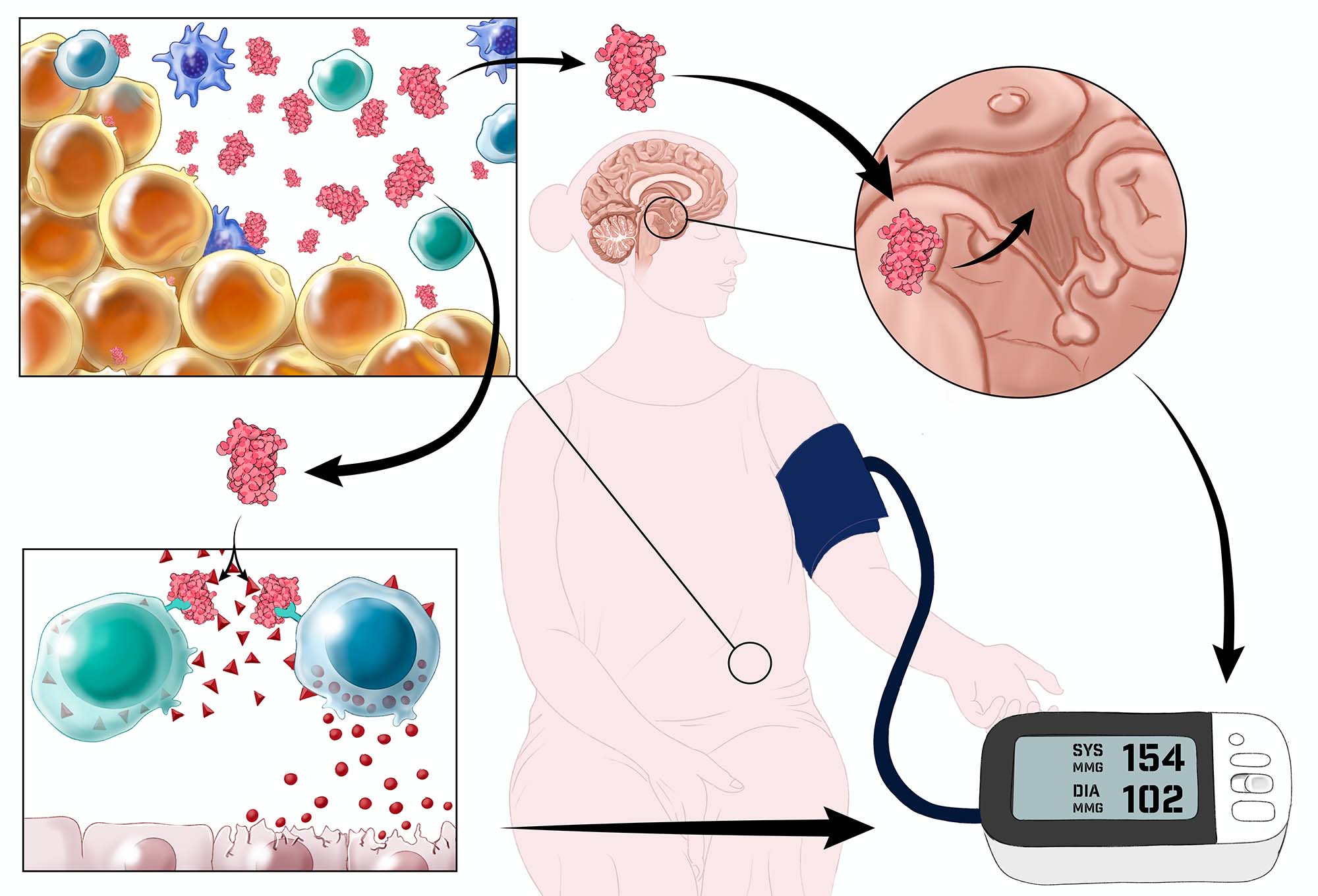
Innate Immune Mediated Changes in Renal Function to Cause Hypertension in Females with Autoimmune Disease
Primary hypertension, or high blood pressure, has been linked to immune system changes similar to those seen in autoimmune diseases. This study explores how the innate immune system contributes to hypertension in systemic lupus erythematosus (SLE), an autoimmune disease affecting mostly young women. Previous research showed that female mice with SLE have kidney issues and high blood pressure, which improve with antioxidants.
This project aims to understand how immune responses in SLE cause these kidney problems
and high blood pressure by investigating a cycle involving immune cell structures called NETs that increase
cell stress and reactive oxygen species (ROS) in the kidneys, leading to worse kidney
function and higher blood pressure. The study will test these ideas and analyze clinical
data from 32,000 SLE patients to find links between inflammation, treatments, and
blood pressure. View Full Graphic Abstract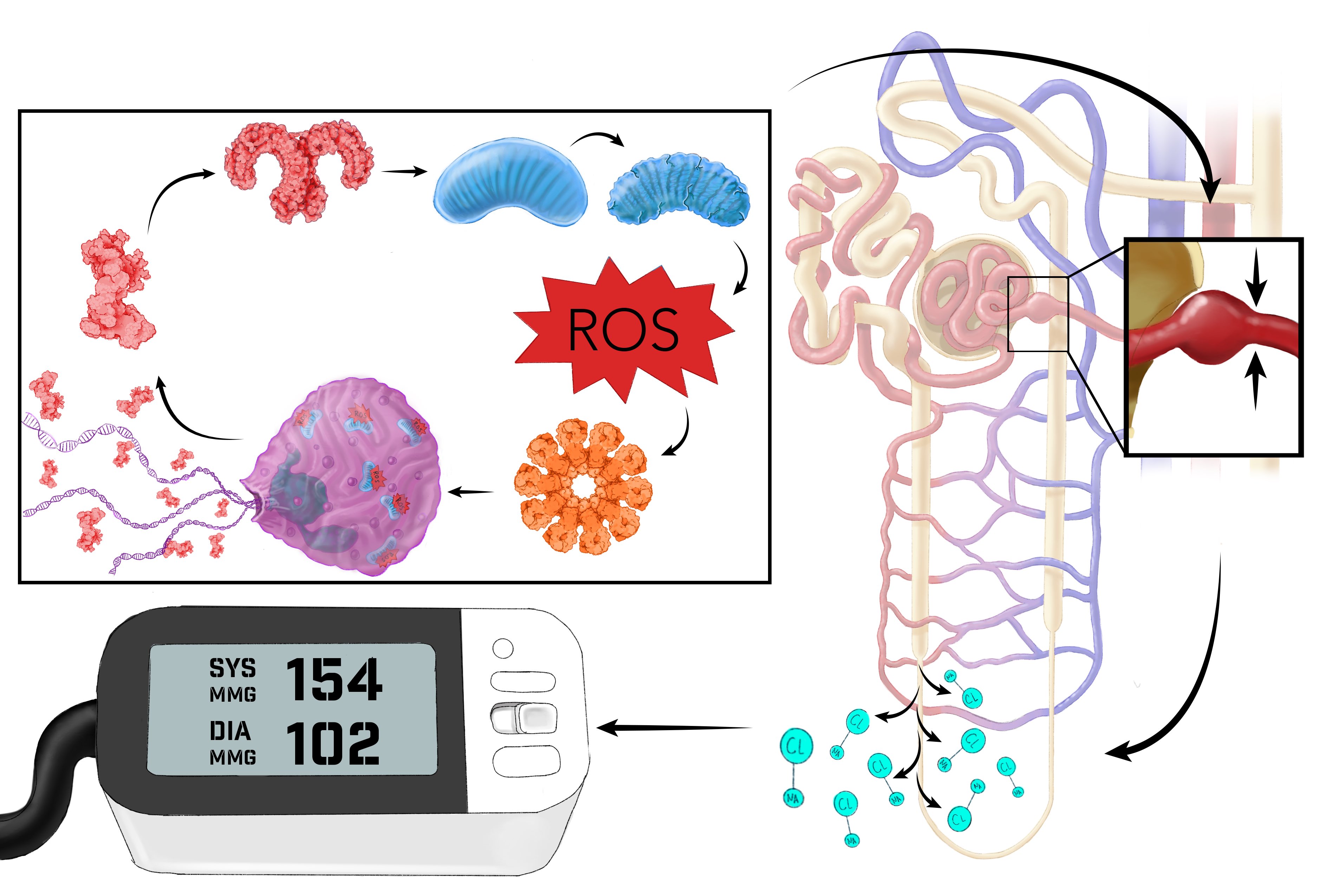
Research Opportunities
To further develop a research pipeline of biomedical scientists trained in Sex As a Biological Variable (SABV) in Cardiovascular Disease (CVD), research and training opportunities are available for researchers at various stages in their careers. For more information on programs, mini-sabbaticals, mentoring, pilot grants, and workshops, please visit our Training page.